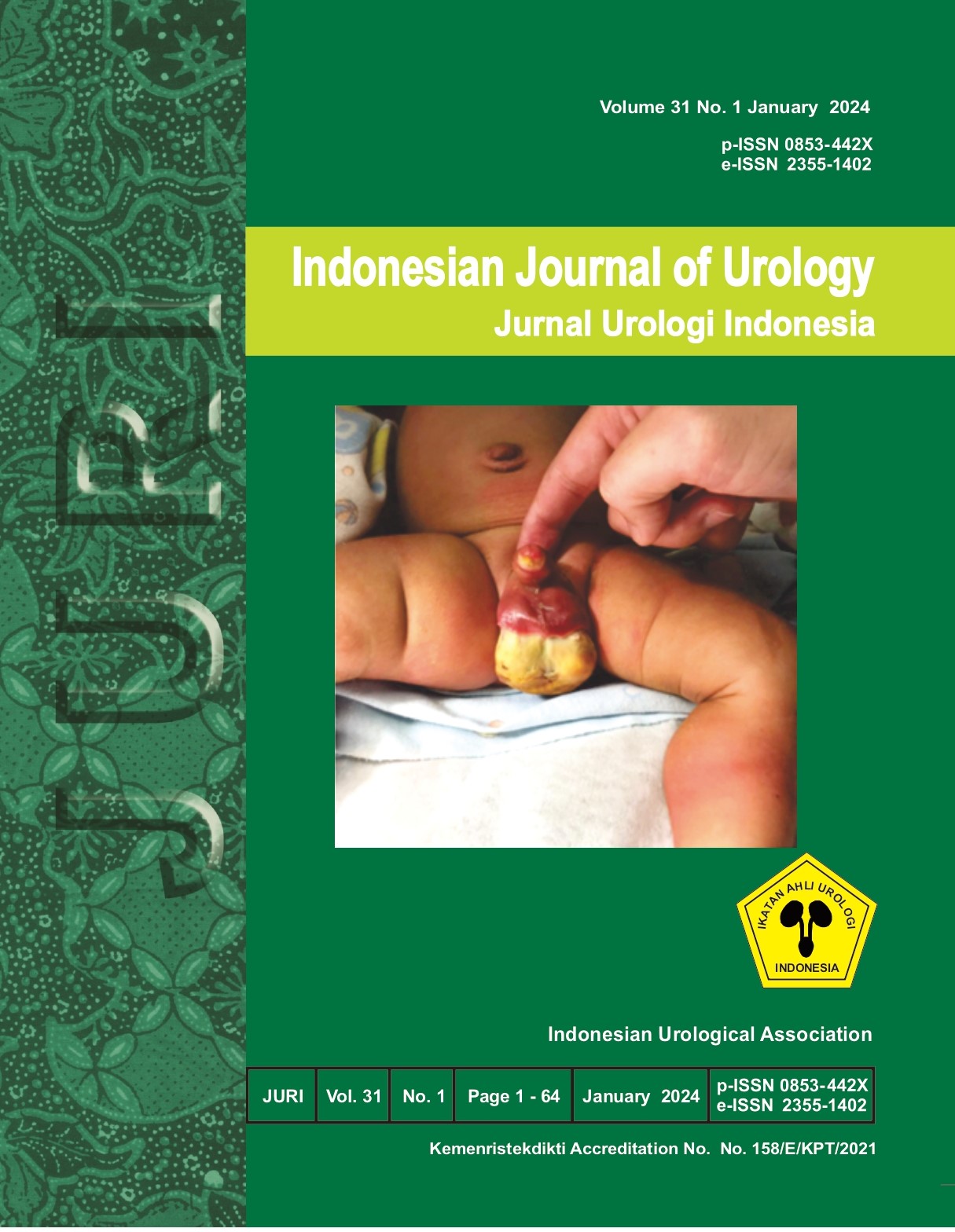
GIANT HYDRONEPHROSIS DUE TO URETEROPELVIC JUNCTION STENOSIS IN PEDIATRICS: A RARE CASE
##plugins.themes.bootstrap3.article.main##
##plugins.themes.bootstrap3.article.sidebar##
Abstract
Objective: This case report presented giant hydronephrosis (GH) due to Ureteropelvic Junction Stenosis in pediatrics. Case(s) Presentation: A three-year-old boy was admitted with abdominal distension and pain for the last three month. CT scan without contrast of the abdomen showed a left kidney size of 141x 97x 63.5 mm, massive dilatation of the pelvicalyceal system, thinning cortex in the left kidney, and left ureter measurement of 16 mm in diameter. An urgent percutaneous nephrostomy tube (10Fr) was placed in the left kidney for this patient, followed by a pyeloplasty procedure in the next three weeks. The patient was discharged on day five, and the six-month follow-up results were good. Discussion: Giant Hydronephrosis is a rare entity, with less than 500 global cases reported in the literature. The diagnostic approach to suspected hydronephrosis in pediatrics is sonography and may be followed by CT or MRI. Management of giant hydronephrosis requires two stages procedure with percutaneous nephrostomy followed by pyeloplasty. This two-stage method ensure the renal function is preserved. Conclusion: Ureteropelvic Junction Stenosis is a common cause of giant hydronephrosis in pediatrics. Appropriate physical examination and other diagnostic approaches are needed to diagnose patients with giant hydronephrosis and determine the best management. Keywords: Giant hydronephrosis, ureteropelvic junction stenosis, pyeloplasty.
##plugins.themes.bootstrap3.article.details##
Giant hydronephrosis, ureteropelvic junction stenosis, pyeloplasty
Kaura KS, Kumar M, Sokhal AK, Gupta AK, Purkait B, Saini D, et al. Giant hydronephrosis: still a reality!. Turk J Urol. 2017; 43: 337-44.
Budigi B, Dyer RB. Giant" hydronephrosis. Abdom Radiol (NY). 2019; 44(5): 1946-1948.
Naim HM, Daryanto B, Nurhadi P. Profile of Pediatric Hydronephrosis in Saiful Anwar General Hospital, Malang, Indonesia. Indian Journal of Forensic Medicine & Toxicology. 2021; 15(3).
Hu G, Luo M, Xu Y. Giant hydronephrosis secondary to ureteropelvic junction obstruction in adults: report of a case and review of literatures. Int J Clin Exp Med. 2015; 8(3): 4715–4717.
Yapanoglu T, Alper F, Ozbey I, Aksoy Y, Demirel A. Giant Hydronephrosis Mimicking an Intraabdominal Mass. Turk J Med Sci. 2007; 37(3): 177-179.
Kamath SP, Ganesh Pai K, Baliga BS. Bilateral Giant Hydronephrosis in a Ten-Year-Old Male. Case Rep Pediatr. 2018: 2470369.
Alsunbul A, Alzahrani T, Binjawhar A, Aldughiman A, El-Tholoth HS, Alzahrani A, Alakrash H. Giant hydronephrosis management in the Era of minimally invasive surgery: A case series. Int J Surg Case Rep. 2020; 75: 513-516.
Sharma U, Yadav S.S, Tomar V. Factors influencing recoverability of renal function after urinary diversion through percutaneous nephrostomy. Urol Ann. 2015; 7(4): 499-503.
Augustin G, Zupancic B, Zupancic V, Visnjic S. Calyceal plication with Anderson-Hynes pyeloplasty in a 7- year-old boy with giant hydronephrosis of a single right kidney. European Journal of Pediatric Surgery. 2009; 19(4): 255–257.
Dino MS, Hassen SM, Tufa TH. Unilateral Giant Hydronephrosis Secondary to Ureteropelvic Junction Obstruction in a Middle-Aged Woman. Case Reports in Urology. 2021: 1.